New "electronic skin" technology is expected to improve the five-year survival rate of patients with chronic wounds
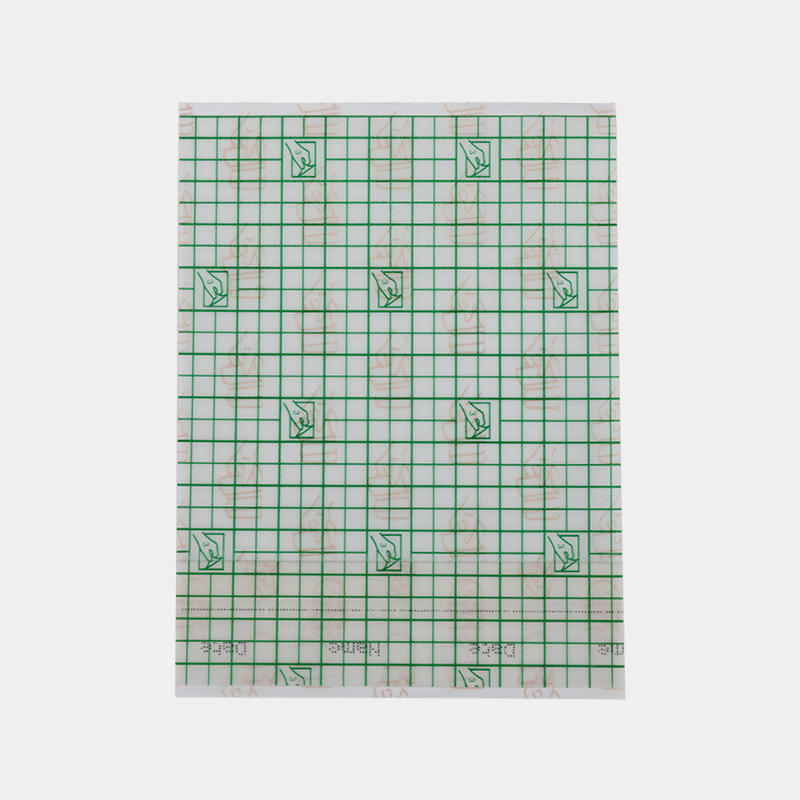
With a major breakthrough in chronic wound treatment technology, a team of researchers from the Keck School of Medicine of USC and Caltech are a medical revolution. The smart bandage technology they developed can not only automatically sense changes inside the wound, but also provide drugs or other treatments in real-time, which is expected to completely change the status quo of chronic wound care.
Improved survival rate and reduced economic burden
Chronic wounds, including diabetic ulcers, surgical wounds, and pressure sores, have long been a medical problem. These wounds not only have a low survival rate but are also extremely expensive to treat, costing as much as $28 billion per year in the United States alone. However, this situation is about to change with the advent of smart bandage technology.
Smart bandage technology
In a review published in the journal Nature Materials, the research team detailed the smart bandage technology. These high-tech dressings are able to provide continuous data on wound healing and potential complications, including infection or abnormal inflammation, and can deliver treatment in real-time. The technology, supported in part by the National Institutes of Health, has been tested in animal models as a proof of concept with promising results.
Interdisciplinary collaboration
This research by the USC-Caltech team is the result of new breakthroughs in materials science, nanotechnology, digital health, and more. Dr. Wei Gao, assistant professor of medical engineering at Caltech and co-senior author of the paper, said the next generation of smart bandages they are developing will be able to wirelessly monitor key metabolic and inflammatory biomarkers in wound fluid.
Regulatory Approval and Commercialization Outlook
Despite the promise of smart bandage technology, there are still several hurdles to overcome before it can be incorporated into standard medical practice. These include changes in the healthcare system's approach to wound care and regulatory approval from the U.S. Food and Drug Administration (FDA). David G. Armstrong, MD, professor of surgery and neurosurgery at the Keck School of Medicine of the University of Southern California, stressed that integrating smart bandages would require significant changes to current standards and would have to make sense to colleagues at the FDA.

Future Outlook
The development of smart bandage technology is expected to not only improve the five-year survival rate of patients with chronic wounds but also reduce the economic burden and improve the quality of life of patients. Dr. Armstrong and his team are studying the use of ultrasound technology to guide the implementation of gene therapy to reduce the risk of amputation in patients with leg ulcers.

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体













.jpg.png?imageView2/2/format/jp2)
.jpg.png?imageView2/2/format/jp2)


