Pressure sores, also known as bedsores, are caused by long-term pressure on the part of the body, which affects blood circulation and leads to tissue necrosis caused by a lack of nutrition in the skin and subcutaneous tissue. They often occur in comatose and paralyzed patients who have been bedridden for a long time and in a fixed position. The skin appears pale, grayish white, or bluish-red, with mild edema, clear boundaries, and conscious numbness or tenderness. As the disease progresses, the skin turns black and purple, and blisters and ulcers appear, even deep into the subcutaneous tissue, muscles, and bones. Understanding these links is crucial to the prevention and treatment of bedsores.

The first part: Compression and blood circulation disorders
The formation of bedsores usually begins when a part of the body is under pressure for a long time, such as the sacrum or heels, which hinders local blood circulation. Obstructed blood circulation means that local tissues cannot get enough oxygen and nutrients, and metabolic waste cannot be effectively discharged, resulting in tissue ischemia and hypoxia.
The second part: tissue ischemia and hypoxia
Ischemia and hypoxia lead to impaired cell metabolism, which gradually causes the cells to lose activity and become edematous and degenerate. Over time, these changes may lead to tissue necrosis, especially subcutaneous tissue, which is more vulnerable than the epidermis.
The third stage: inflammation and exudation
After tissue necrosis, local inflammatory reactions will occur. Inflammatory cells such as white blood cells and macrophages infiltrate around the necrotic tissue and release inflammatory factors. The inflammatory response causes increased vascular permeability and components such as plasma and proteins seep into the interstitial space to form exudate.
The fourth stage: blisters and ulcers
As the exudate increases, blisters may form under the skin. The blisters may be small at first, but as the disease progresses, they may gradually increase in size and rupture. When the blisters rupture, the protective layer on the surface of the skin is destroyed, exposing the necrotic tissue underneath, which is prone to forming ulcers.
The fifth stage: infection and spread
After an ulcer forms, local tissue loses its protection and is vulnerable to bacterial invasion. Bacteria multiply in necrotic tissue and exudate, causing infection. The infection may spread to surrounding and deep tissues. In severe cases, bacteria may enter the blood circulation and cause systemic infections such as sepsis.
The sixth step: is tissue repair and scar formation
When a bedsore develops, the body automatically begins to repair the damaged skin and tissue. During the repair process, the body grows new blood vessels, cells, and collagen to fill the damaged area. Scars may form if the bedsore is severe or the repair process is disturbed (such as infection, inflammation, etc.).
How to prevent it?
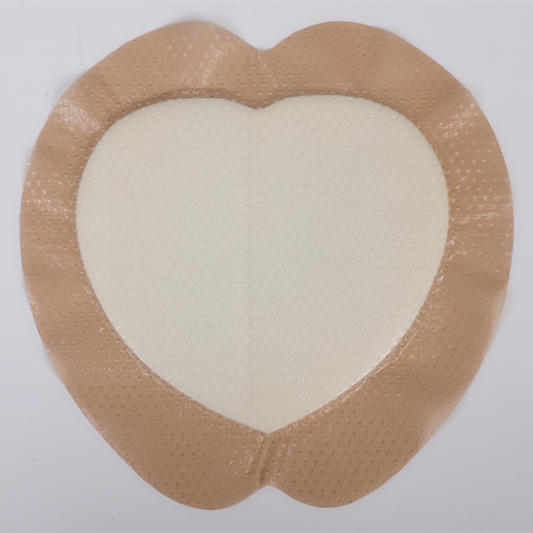
For patients who are bedridden for a long time, you can use pressure relief silicone gel foam dressings, cushions, and other devices to reduce local skin pressure. These devices can reduce the occurrence of bedsores by dispersing pressure and providing air circulation. When choosing pressure relief devices, you should choose according to the specific situation of the patient to ensure the comfort and effectiveness of the equipment.
Balanced diet Provide a diet rich in protein, vitamins, and minerals, and adjust the diet plan according to the health status of the elderly. Water intake: Ensure adequate water intake to prevent dehydration. For the elderly who have difficulty eating on their own, patient feeding is required to ensure that their nutritional needs are met.
Regular turning and body position adjustment: once every two hours to relieve pressure on specific body parts. Use professional nursing pads and mattresses: Use anti-pressure sore mattresses or gel, air cushions to relieve pressure. Skincare: Keep the skin dry and regularly check for potential signs of pressure sores, such as redness, swelling, or damage.
The formation of bedsores is a multi-factor, multi-link process. By understanding these links, we can more effectively prevent and treat bedsores and improve the quality of life of patients. For more information on Innomed®Silicone Foam Dressing, Refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








