An acute attack of chronic heart failure (CHF) is fluid retention caused by cardiac volume overload, which causes organ congestion and subcutaneous tissue edema. Patients often present with dyspnea, fatigue, pulmonary congestion, and limb Symptoms such as edema. Lower extremity ulcers refer to chronic skin ulcers that occur in the lower legs and ankles and are more common in the elderly, especially those with vasculitis, diabetes, and lower extremity venous return disorders. Risk factors include venous insufficiency, peripheral arterial disease, obesity, phlebitis, and other factors such as heart failure. Heart failure is one of the most common reasons for hospitalization and readmission in older adults. While we generally don't think of it as a potential trigger for leg wounds, the reality is that it is a common cause of leg ulcers developing or worsening. Usually, the elderly is more common and often have a variety of chronic diseases (hypertension, diabetes, coronary heart disease, etc.) The literature has reported that severe subcutaneous edema caused by ACHF can cause ulcers and persist for a long time.
Why does heart failure cause leg wounds?
Peripheral edema is a typical sign of congestive heart failure and can rapidly develop during episodes of decompensation. Bilateral edema is often associated with obesity, venous thrombosis, or hypoalbuminemia. This edema may be related to left or right ventricular dysfunction, with autoregulatory mechanisms of the cardiovascular system, and simultaneous fluid retention is related to the medications used to treat it. In patients with right heart failure, bruising occurs with swelling and peripheral fluid accumulation. In left heart failure, the increase in cardiac output, in addition to its possible effect on the worsening of proper heart function, activates compensatory mechanisms (neural and hormonal) that cause the action of the renin-angiotensin system along with peripheral edema due to retention of sodium and water. The space between capillaries and tissue increases whenever there is edema in the legs, regardless of the cause. This makes it more difficult for nutrients to diffuse, reducing skin perfusion. Thus, especially in patients with arteriosclerosis or venous edema, perfusion may become insufficient, and ischemia and skin necrosis may occur if the perfusion is already deficient. In addition, fluid accumulation in the legs means the possibility of skin stretching and separation at the dermo-epidermal junction, with the appearance of cracks, erosions, or blisters. This effect is more severe in patients with sarcopenia, where skin tears are more likely to occur. It is not uncommon for Martorell ulcers (subcutaneous ischemic small arteriosclerotic ulcers) or arterial ulcers to appear for the first time after the onset of decompensated heart failure. On the other hand, cardiac insufficiency is considered a risk factor for venous ulcers.
Since heart failure is a typical syndrome in the elderly, it is not uncommon for the same individual to have some degree of arterial/arteriole disease, chronic venous and lymphatic insufficiency, and cutaneous laxity, which increases the risk of chronic ulceration.
How do you deal with these wounds?
After correcting cardiac decompensation, the wound is staged according to the degree of wound and exudate to select dressings. Patients with a wound infection can use a new type of silver-containing silver ion dressing, which can effectively protect the wound surface. It will not cause pain and granulation tissue damage and has an excellent bactericidal effect. At the same time, it can prevent and treat wound infection and effectively protect the new granulation tissue.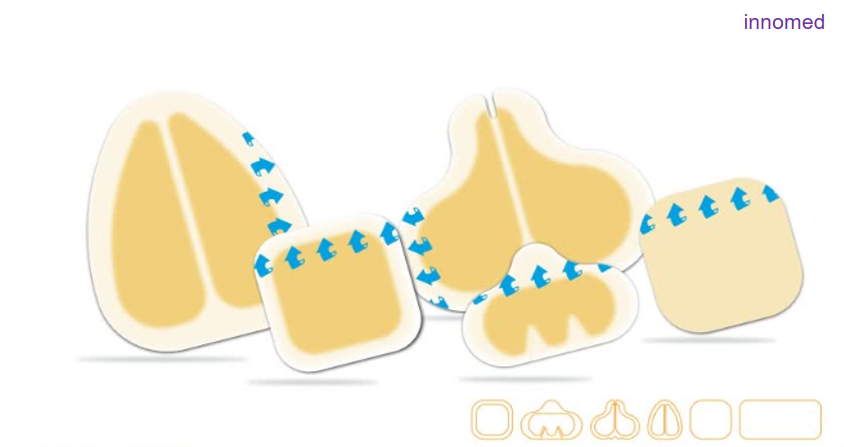
How to use the dressing:
Cover the wound with the cut dressing and use a self-adhesive medical bandage to fix it. Alginate dressings can also be used if a small amount of blood oozes from the wound after debridement. Alginate has a hemostatic effect and will form a gel after contact with exudate, which can absorb a moderate to a large amount of exudate, keep the moist wound environment, conform to the contour of the wound bed, and promote the wound to crawl. The outer dressing continued to use hydrocolloids. Change the dressing daily, closely observe the exudation of the wound dressing, and change the external dressing in time.
Patients should note:
Pay attention to anti-edema measures (elevate the legs to rest) and activate the muscles with ankle dorsiflexion and plantar flexion exercises, even in patients with limited mobility. These measures are also crucial in terms of prevention and are related to proper monitoring and control of heart failure. Considering that these individuals are usually older, with venous edema or fragile skin, we suggest that self-adhesive bandages are best used to regulate the pressure system.
For more information on Innomed® dressings, refer to the previous articles. If you have customized needs, you are welcome to contact us; we will serve you wholeheartedly.
At Longterm Medical, we transform this data by innovating and developing products that make life easier for those who need loving care.
references:
1. Urbanek, T., Juśko, M., & Kuczmik, W. (2020). Compression therapy for leg edema in patients with heart failure. ESC Heart Failure, 7, 2012 – 2020.
2. Augey F, Pinet A, Renaudier P. Insuffisance cardiaque et ulcère de stase : une association significative (étude prospective de 100 cas) [Heart failure and stasis ulcer: A significant association (prospective study of 100 cases)]. Ann Dermatol Venereol. 2010 May;137(5):353-8.
3. Saucedo D, Evans N, Lim CS. Initiating compression therapy for those living with heart failure. Br J Community Nurs. 2021 Sep 1;26(Sup9): S12-S17.
Editor: kiki Jia
Date: July 5, 2022

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








